
Special Article 2, Issue 10.2
Perspectives on Getting Dental Team Members Involved in DSM
http://dx.doi.org/10.15331/jdsm.7294Disclaimer: The use, mention or depiction of any product, device, service or appliance shall not be interpreted as an endorsement, recommendation or preference by the AADSM. Any opinion expressed is solely the opinion of the individual, and not that of the AADSM.
As every dentist knows, having good staff can be critical in having a thriving practice. Office managers, dental assistants, hygienists and other patient-facing team members are often the patient’s first and most frequent point of contact. For a practice that is dental sleep medicine-focused, it becomes even more important to get all staff fully invested in the mission of treating sleep-related breathing disorders. We wanted to hear from team members how dentists can get buy-in from their staff. Here are some of their answers:
HOW CAN DENTISTS ENCOURAGE TEAM MEMBERS TO BE SUPPORTIVE OF THE DSM PART OF THEIR PRACTICES?
“Because your office team spends more time with your patients than you do, successful offices empower team members to build therapeutic relationships with patients. Our goals are to prevent, treat, and resolve the situations patients present every day. This can be accomplished by treating DSM with the same focus as all other areas of our practice.
Investing time and finances in your team’s education and chairside tools is a first step toward successfully building DSM into your practice. This will ensure that your team is asking the right questions for sleep and airway as part of every health history, as well as the ability to discuss the answers with the patient.
As an example, your dental hygienist is confident in recognizing and discussing periodontal treatment with passion because he/she believes and is confident about this area of dentistry. Conversely, when observing a scalloped tongue, evidence of bruxism, dry mouth, or a high vaulted palate, are they clear about an organized approach? This situation could apply to your chairside treatment coordinator or any of your administrative team. Confidence is critical because as we know when the dentist leaves the room, patients are quick to ask team members: “What do you think I should do?”
The bottom line is your team must believe what you believe, have a structured approach and feel confident in articulating those ideas. Finally, you, as the dentist, should express your gratitude to them, for their involvement with the success of the treatment, especially in front of the patient.”
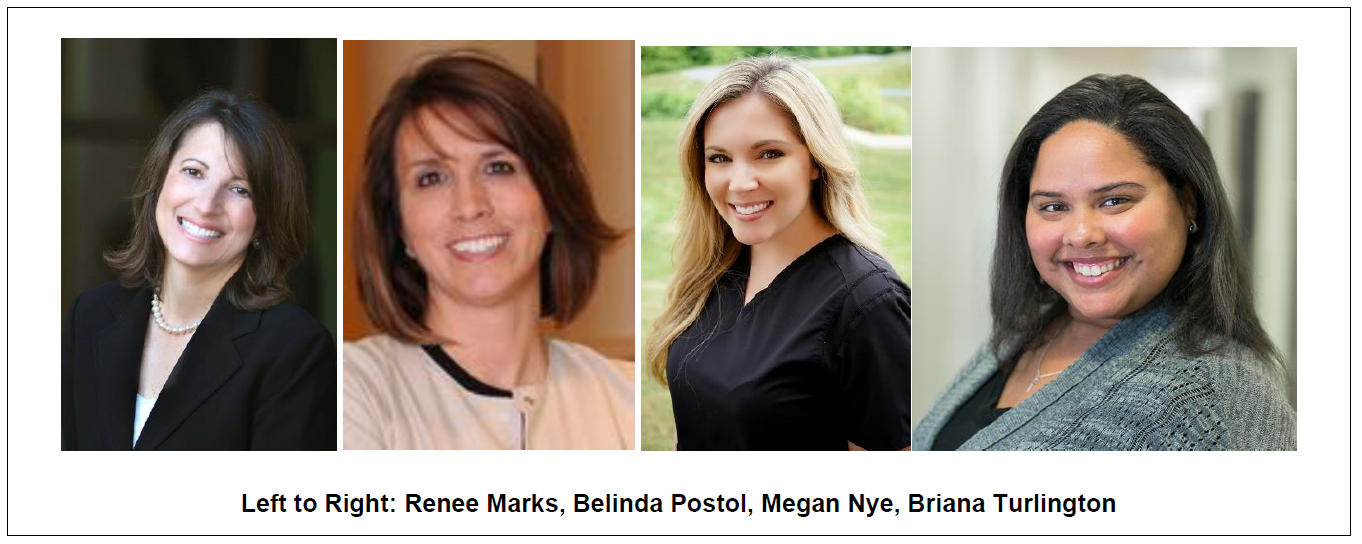
-Renee Marks
“One of the biggest challenges when treating sleep apnea patients is getting dental team members on board and excited. Dental team members are comfortable treating dental patients, and when the additional service of sleep apnea treatment is added, it can cause fear that dental services will be pushed aside. We have found that it is helpful to be very clear on the intent of treatment and how those services fit into your dental practice. The other thing to keep in mind with your team members is what makes them feel secure, challenged and motivated. The best way to meet these needs is to have your team complete a personality assessment. By knowing your team members personality types, you can find the best way to address their needs and make them feel secure and valued in the process. For example, if your staff member has a DISC personality type of D (Dominance), they will respond best to knowing the big picture, including statistics, and will appreciate being challenged to meet certain goals. However, that approach would not work for someone with a DISC personality type of S (Steadiness). They don't respond well to being rushed but are cooperative and loyal and will work hard to please you. It would benefit you to know which of your team members should be in each role and how to motivate them to move forward with your vision.”
“I managed a hybrid office that was mixed with prosthodontics and dental sleep medicine for over a decade, until we merged with a local hospital system, and now I exclusively focus on dental sleep medicine. I think that empowering the team to feel comfortable discussing dental sleep medicine with patients is so beneficial. It can give those team members a different outlook and it helps guide conversations and identify patients within the office that may be suffering with obstructive sleep apnea, but not yet diagnosed. Our provider would take time to review education materials and things that we could look for when screening patients. A topic of discussion on “how retrognathia is an increased risk to develop obstructive sleep apnea,” became a powerful resource to our team.
Our team was able to take this information and identify an untreated patient with retrognathia. While in private practice, we had a patient that who was not a cookie cutter sleep apnea patient: she had a normal BMI, she was active, she was, overall, a very healthy petite patient - but she had a very retrognathic jaw line. With guidance from the provider and prior educational discussions, our team realized that obstructive sleep apnea, resulting from retrognathia, could be playing a part in a number of possible health concerns.
The patient completed a sleep test, and it came back she had obstructive sleep apnea. Our team then assisted this patient in obtaining an oral appliance for treatment and she was able to then see some great health improvements. It was very rewarding to be able to help this patient succeed in her health goals. It is so important to educate our teams to create more conversations with patients that can lead to positive outcomes of treatment.”
“I believe the best way to get team members’ support for DSM within an existing general dentistry practice is to get to the root of any fears the team have. Fear of the unknown, of messing up, or of saying the wrong thing can be debilitating, which in turn, holds the entire practice back. Once the fears are recognized, training and support become integral. Making each team member clear about what they are responsible for, why they were chosen for that specific task and how their role affects the team as a whole is extremely important and empowering.”
What are your thoughts on the new getting your team members more involved? Join the conversation by posting on the AADSM Discussion Board today!
