
Special Article 1, Issue 8.1
Perspectives on Communicating With Patients
http://dx.doi.org/10.15331/jdsm.7184As dentists, communication with patients can be critical to ensuring that patients initiate treatment and comply with their plan of care. For qualified dentists treating sleep-related breathing disorders, communication can be especially crucial as providers navigate issues such as compliance, cost and side effects.
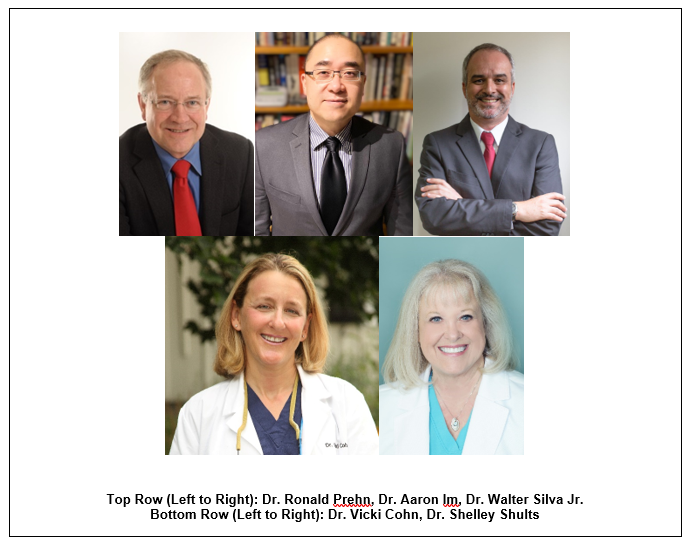
We reached out to several of our American Academy of Dental Sleep Medicine members to ask what their best practices are for communicating with their patients.
HOW DO YOU APPROACH DISCUSSING OSA SCREENING WITH YOUR PATIENTS?
“I ask questions based on comorbidities of OSA. I relate to the patient observations you have from your exam and from their history. I “build a case” based on their answers. Each symptom can be explained away as being caused by something else, but put it all together, it makes the patient become aware.”
-Ronald Prehn, DDS, D.ABDSM
“While sleep bruxism is not always necessarily indicative of sleep-disordered breathing, as a dentist, I find that this topic is a great foot-in-the-door to explore the topics of sleep arousal and sleep fragmentation with the patient. This begins to raise questions and awareness about myofascial pain, TMD, and tooth wear. And then finally the screening appointment organically graduates into a discussion about OSA and its comorbidities. Once the patient begins to identify their own signs and symptoms with everything discussed, they typically leave well-motivated to go get a sleep study.
-Aaron Im, DMD, Qualified Dentist
“OSA has a huge prevalence in the population. In Brazil, my country, a study showed (Tufik, 2010) that roughly 1/3 of adults has OSA. Then, I use specific questionnaires and oximetry for all. Those with suspected OSA (desaturation and/or complaints) are referred to have a sleep study . I always emphasize the enormous problems that come from non-treated OSA. So, I explain all treatments and their benefits. Then, OAT is explained in detail.”
-Walter Silva Jr., DDS, ABDSM International Certificant
“In my previous practice, when I was a general dentist that treated OSA, that discussion did occur. I learned to be judicious about how and when I discussed it. It was fairly easy to see all the “red flags” by looking in their mouth/airway and reviewing their health history, but it did not mean that the patient felt they were in my practice to discuss this.
I would continue with the thorough dental exam and discuss all those issues first, discuss the treatment plan, etc. Then, I would start planting the seed concerning possible OSA – something like, “by the way, how much does your spouse complain about your snoring (if I saw a very long uvula)?”, or “I did notice that you are on 3 medications to control your high blood pressure and now they have you on a med to control you nocturia, etc.” I would then start explaining that it is possible that they have OSA. Sometimes, that discussion would occur at their next visit, so I wasn’t taking up too much hygiene time. For my patients that I had known for many years, it was an easier conversation - for newer ones, it was important to be more tactical. I would then let them know I thought a consultation with a sleep physician would be helpful so that they could determine if a sleep test was advisable. I had created relationships with the surrounding sleep physicians, and I did not expect a “boomerang” relationship where they would always refer the patient back to me for OAT. If they thought CPAP was a better initial choice, I was OK with that – there is enough fall out of CPAP to keep us all busy with OATand we should always be looking to treat our patients optimally using any treatment that helps them. AND, if you do not have that philosophy, your community physicians will figure it out and they will not refer to you.”
-Vicki Cohn, DDS, D.ABDSM
“The most opportune time to discuss OSA for my practice is during the routine examination…As I see findings of concern, I’ll mention them to the hygienist or scribe and let the patient know I will explain my findings after completing the exam. Remember that when the patient is in your hygiene chair, their focus is on dental findings, so you must first be thorough in your dental examination/presentation and report dental findings first. As an astute provider that has identified an airway concern, you must also consider the patient’s personality, demeanor, and readiness for discussing health concerns outside of what they perceive is “only a dental appointment”.
An easy opening for OSA discussion is to ask the patient questions regarding their health, sleep quality, sleep habits, snoring, insomnia, gasping, etc. Give them a chance to engage in the topic. Ask if they have ever heard of or have any interest in learning more about a potentially harmful medical condition called obstructive sleep apnea that they may need tested for? Frequently, they are very interested in treating their snoring or sleep issues and this is a conversation starter…
You or your staff are now able to educate the patient on your findings and concerns and introduce them into the field of sleep medicine. Yes, I said sleep medicine, not instantly dental sleep medicine. The diagnosis and prescriptive choice is unknown at this time. We should desire a treatment modality that is most appropriate for our patients and provide them with appropriate choices utilizing a multidisciplinary team approach. An informed patient who is in involved with ownership and management of their own condition is a much happier, more successful and most compliant patient.
I mention that there are several forms of sleep apnea treatment available. Oral appliance therapy is briefly mentioned to help them realize that it is one of several treatment modalities, depending upon many factors. Time management is often challenging with positive findings. This is a good time to simplify the discussion that explains the steps of screening, referral, diagnosis, modalities of treatment, expectations and if appropriate, potential insurance coverage so patients are not overwhelmed. I focus the conversation in directing the importance for initial accurate diagnosis and treatment planning between providers that is patient focused.
A customized brochure may be given to the patient to transition your discussion. Refer the patient to visit your DSM website for further information. Staff appreciate the opportunity to educate about DSM and OSA! At this point, your trained staff can continue the conversation and assist in scheduling the screening test or making the sleep physician referral...”
-Shelley Shults, CPN, MSN, DDS, DABDSM
HOW DO YOU DISCUSS THE VALUE OF OAT WITH YOUR PATIENTS?
“First, one has to get the patient to value treating OSA. I use subjective symptoms and objective testing to get them to understand they have a problem, then I talk to them about consequences. As I review treatment options, the OAT option is obviously the one preferred almost every time!”
-Ronald Prehn, DDS, D.ABDSM
“After they know the importance of treatment, I explain more about OAT. Its types, materials and outcomes are showed based on clinics cases that were performed.”
-Walter Silva Jr., DDS, ABDSM International Certificant
“I talk about all treatment forms (including surgical treatments) with my patients. I focus more on CPAP, as it is the most well-known form of treatment and the gold standard. I explain why it is the gold standard - because it has great efficacy and it is the only non-site specific treatment for OSA. I also explain that it is very difficult to use and help them understand that just because they may have failed CPAP, it does not mean they are “losers” – 50% of patients that try CPAP cannot sleep with it. I then explain how OAT works and how it compares in efficacy to CPAP, but I also tell them that literature and my clinical experience shows more patients can tolerate OAT – a lot more! I let them know that it is the next best non-surgical approach to treat their OSA. Bottom line, I give them facts so they can make their own judgement. I always let them know I can never give them an iron clad guarantee OAT will work for them. If I think they are a challenging candidate, I will tell them.”
-Vicki Cohn, DDS, D.ABDSM
When I think of discussing the value of OAT, I think of the phrase “beauty is in the eye of the beholder.” The perception of beauty is subjective and it gives perceived value. If the patient can perceive the treatment modality as therapy for increasing quality and quantity of life, then the value is greater.
Regarding the patient who is CPAP intolerant, they usually have experienced the ongoing costs of PAP therapy and are pleased to have a definitive disclosed dollar amount revealed up front when considering oral appliance therapy. Regarding objective value from specific appliances, I use premium appliances with longer warranties and this adds monetary value to oral appliance therapy.
I discuss potential of side effects and how we minimize such with milled appliances, jaw exercises and morning re-programmers. For the patients who are interested evidence-based findings, I provide several pages of notated research articles in a presentation folder that they can study. We also have included handouts regarding systemic and social dangers of untreated OSA.”
-Shelley Shults, CPN, MSN, DDS, D.ABDSM
WHAT ARE THE MORE DIFFICULT ISSUES TO DISCUSS WITH PATIENTS? HOW DO YOU APPROACH THESE TOPICS?
“Compliance. [I approach these topics] [s]everal ways depending on the type of person I am talking to. Some like to hear how they will feel better or live longer. Some like to see “evidence” - so for those, I use pulse oximetry to show them the improvement with OAT and especially the effect on the heart (which is the silent killer for these patients).”
-Ronald Prehn, DDS, D.ABDSM
“With obesity increasing both the risk and consequences of OSA, weight management can be an important part of OSA treatment. No one likes to be told they need to lose weight and some may even feel insulted or defeated when this topic surfaces during treatment, especially when they’ve heard the same thing from multiple treating doctors. Rather than focusing on the negatives of weight gain itself, I speak positively on how much more powerful our oral appliance therapy can become with any amount of weight loss. This approach is much more incentivizing and less condemning to our obese OSA patients.”
-Aaron Im, DMD, Qualified Dentist
“I think that first consultation, with a lot of explanation about the disease and the importance of treatment, is quite useful. If you do not do this, you will have trouble and, in some cases, if you don’t "touch" the patients, they won’t accept treatment. The broader your approach, the more aware patients will be. So, they will want to improve their health.”
-Walter Silva Jr., DDS, ABDSM International Certificant
“I’m a straight shooter – I tell them about common OAT side effects from the beginning, admittedly near the end of the consult (do not start the conversation with that – give them the advantages first). I want there to be a common understanding of what to expect or what might happen. It’s in my informed consent. It’s definitely easier in a referral-based practice like mine, as patients have come to me because they are seeking a solution to their poor sleep and probably have been for a while before they get to me. In a general practice, they may not yet understand that they are experiencing poor sleep, or they may think it is due to multiple other things. Additionally, they probably haven’t associated it with their sleep apnea yet. As a general practitioner, I think you need to discuss your desire to help your patients become optimally healthy by treating their OSA. If you want your patients to know that you care about them, let them know that you don’t care whether they choose CPAP or OAT to treat their OSA and you just want them to get treated – half will fail CPAP and come running back to you anyway – but you will be doing the right thing and gaining a great deal of trust from your patients. They will think you are wonderful and will continue to place their trust in you for all of their oral care. It will be a win-win experience for everyone.”
-Vicki Cohn, DDS, D.ABDSM
“My most difficult issue is approaching the ‘same and similar’ clause with Medicare patients who require combination therapy of OA and CPAP but received CPAP prior to OAT. Patients (and providers) do not understand the general application of this clause when it clearly would benefit the patient’s health. I attempt to educate my referring providers, if appropriate in their eyes, to prescribe OAT before CPAP to Medicare patients, especially if they have mild to moderate OSA or they refuse or are intolerant to PAP therapy. They would then be able to use combination therapy...
The most disappointing issue for me is discussing incomplete or non-response to OAT with a patient. During my initial consultation with the patient and in the consent agreement, we have discussed the potential for partial or complete non-response to OAT. I demonstrate the various types of obstructions and describe the potential for incomplete or non-response. I have never had a patient upset with me personally who did not respond, only disappointed and some that continued to wear the appliance despite insufficient response. We send thorough documentation and records to expedite the alternative therapy referrals. We follow-up periodically to for updates.
A disappointing and difficult issue is addressing the long-term side effects of dental change when the patient has not been compliant in follow-up visits, TMJ exercises, wearing of the re-programmer, or accepting the warning of potential occlusion changes. I have several approaches to the long-term side effect management, primarily dental change and very rarely, long-term disc dysfunction or displacement. Document, document, document from the start. Take photos and keep models/scans. Recheck ROM changes at periodic recheck appointments. Prevention is the best treatment. It is difficult if not impossible to reverse most of these changes. Be ready to accept a change in treatment modality if the patient is intolerant or displeased with physical changes. Teach the patient to monitor their bite in the mirror weekly.”
-Shelley Shults, CPN, MSN, DDS, D.ABDSM
